Template File: /www/wp-content/themes/stn2017/single.php | Template Hierarchy
WP version: 6.4.4
PHP version 8.2.17
Paediatric trauma pathways in the NoSTN have been rolled out and developed since August 2019 across Grampian and Highland.
Over this time, service improvement projects have been carried out to improve delivery of care to these patients. Of significance are the number of patients to benefit from the trauma pathway within RACH who do not meet STAG inclusion criteria. The trauma pathway, which includes psychology and trauma coordinator input alongside relevant specialties and therapies, has allowed for a greater cohort of patients to access enhanced care following a traumatic injury. Services have also been extended to include burns patients where appropriate. We continue to promote our service and pathway by regular face to face promotion and posters throughout RACH to ensure familiarity and an easy referral process for staff.
Data collected for RACH between August 2019 and June 2022 shows that 89 patients have been commenced on the trauma pathway. Of those, 22 patients did not meet STAG inclusion criteria. This equates to roughly 25% of all patients. Comparison of both patient groups shows similar mechanisms of injury and patient/family needs following injury, further justifying the need for inclusion of patients out with audit criteria. Data shows that accidents involving motor vehicles and falls from height were the most common cause of traumatic injury. Numbers are also currently being collected to identify how many patients required psychology input following traumatic injury, with or without a rehab need. The intention has always been to improve patient care for all patient groups by creating a robust pathway which can be replicated. These figures highlight the far reaching benefits of this pathway, showing that clinical reasoning for individual cases ensures the most appropriate patients are encompassed.
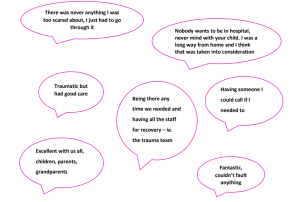
Patient experience questionnaires have been developed for paediatric patients and their families. There are 3 different questionnaires aimed at 7-11 year olds, 12+ years and parents/carers. These are designed to gain positive feedback regarding service delivery as well as to identify areas of improvement. Comments received from recently completed questionnaires are below:
The paediatric trauma coordinator role recently adapted to include cross working over paediatric and adults MTCs. There have been many advantages to this. When an adult is admitted to hospital, their children’s lives are significantly disrupted. The child may not directly be involved in the trauma themselves. However, the dual role enables additional areas of support to be highlighted and provided for these families. Following education for adult colleagues, there is an increased awareness of child protection concerns. Links with paediatric services are now stronger and more efficient. There are times when a child/children and adult/s from the same family are admitted simultaneously. Having links with both hospitals enables smooth communication and visiting, joined up care and a consistent point of contact for the family. There is also a group of young people who may fall under adult services but whose needs very much lie within paediatric services. This can be dependent on age and stage, whether they are still a dependent living at home and whether they still attend school. Strong links with both teams ensures these patients have access to the appropriate professionals and that links can be made with schools/nurseries, families and third parties to ensure tailored support.
CBIT in Hand
We have recently established excellent links with our colleagues at the Child Brain Injury Trust. As a result, we have joined forces and launched the CBIT in hand app in RACH. This app is designed to provide information and advice following head injury to patients and families, professionals and third parties who come into contact with the child. Head injury may range from mild concussion through to traumatic brain injury. The app has been well received throughout the hospital by staff and patients alike. Details are being collected of those signposted to the app in order to gain feedback.
RACH Website
During the 2020 Covid pandemic, patients were contacted to gain information on preferred communication methods and access to information/resources. The responses overwhelmingly pointed to the need for online, electronic and easily accessible information. This was true from both patient and parent perspectives. It was identified that a platform for sharing such information was missing. Following research and networking around the hospital, it was found that this was a widely supported idea. Fast forward a few years and we are in the midst of RACH website development, having been lucky enough to secure the support and funding from the Archie Foundation. Once complete, this will feature a section for the Major Trauma Centre, helping to promote the identity of our service and provide easy access to online information for families.
Follow-up Phone Call Audit
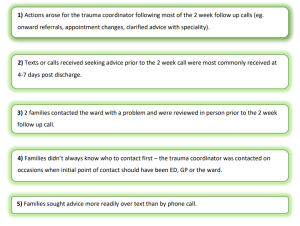
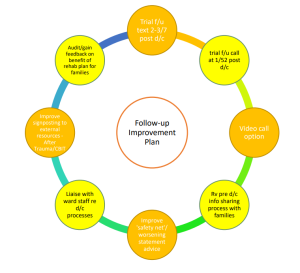
Patients who are commenced on the RACH trauma pathway will receive a follow-up phone call from the trauma coordinator after discharge. The purpose of the call is to provide safety netting, advice and action any outstanding issues which the family may have. An audit was completed to identify potential improvements to the follow up process for paediatric patients. Findings were as follows:
In October 2021 a team from RACH travelled to Orkney to undertake 2 days of paediatric trauma training. This involved lecture based education, multidisciplinary team simulation training with in situ practical procedures as well as question and answer sessions. Topics covered included chest and abdominal trauma, traumatic brain injury as well as child protection concerns and child death. The team thoroughly enjoyed their time there and the feedback was good. A similar trip is planned for September 2022 to Caithness General Hospital.
During Covid, the inpatient responsibility for those with head injuries moved from ED staff to the paediatric general surgeons. To try and ensure consistency with who was being admitted from ED, a proforma was created in accordance with SIGN guidelines. This has meant that decision making about who receives scans, who is observed, who is admitted etc is more streamlined and has led to clearer communication between the ED team and general surgery staff who look after these patients on the ward. The document has now been in circulation for over a year and we are looking at auditing its compliance in the near future. The remote and rural sites across the North of Scotland have also adopted this document. A similar inpatient proforma is also in circulation.
TRiM (Trauma Risk Management) is a trauma-focused peer support system developed to provide early help and information to staff who have experienced a traumatic/adverse/distressing event. Staff working in major trauma settings can be affected by a single distressing event or an accumulation of difficult/challenging situations. Indeed, this is relevant to working in a hospital setting more broadly and certainly not limited to major trauma. Enhanced staff support structures have been developed within RACH (and across NHSG) over the last few years. TRiM is one such development with an established pathway to request TRiM input following adverse events. Funding provided by the NoS Trauma Network enabled the Clinical Psychologist within the MTC pathway to complete TRiM training (practitioner and TRiM manager training) and contribute to the TRiM support available across RACH.
Written by Nina Currie (Paediatric Trauma Coordinator), Ashley Allan (Clinical Psychologist), Gillian Winter (Paediatric MTC Lead NoS/Specialty Doctor